All of us see patients who have tonsillitis or pharyngitis that is clearly more than the “run of the mill” sore throat, but what specifically is wrong and how should they be treated? Although most of you are aware of these conditions, we thought presenting them in an organized fashion may help you to diagnose, treat and refer these patients more efficiently and effectively. Of course, not all patients read the textbook before becoming ill!
Peritonsillar Abscess (PTA) typically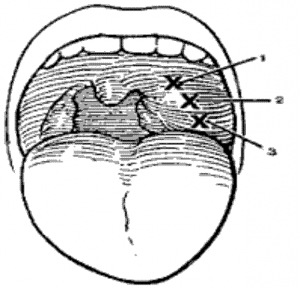 presents with several days of sore throat which has become dramatically worse over the last 24 to 48 hours. The patient has trouble swallowing even liquids and has a “hot potato” voice. On examination there is a moderate amount of trismus making it difficult to open the mouth. The uvula is swollen and displaced to the opposite side. The anterior tonsillar pillar is classically quite swollen and hides most of the involved tonsil which may have some exudate. The contralateral tonsil usuallyappears normal. If a CBC has been done, white cell counts are elevated and there is a left shift. A diagnosis is made when aspirating the peritonsillar space yields frank pus. This procedure is done by spraying the pharynx with topical anesthetic and then injecting the upper outer mucosa (X) and underlying space with stock solution of 1% xylocaine 1:100,000 epineprine. About 3 to 5 mls are used. After waiting about five minutes the peritonsillar space is then aspirated with an 18G needle on a 5 or 10 syringe. Often times in an ER setting this aspiration will provide temporary relief until more definitive drainage can be done. Once the abscess is drained the patient can usually be managed on oral p medications and antibiotics (penicillins or erythromycins) as an outpatient. The chance of developing a second PTA or going on to have chronic tonsil problems is about 15%. Therefore, we usually do not recommend a tonsillectomy un the patient has a second abscess or significant prior tonsillar problems. Tonsillectomy at the time of abscess drainage i usually avoided as the patient needs a general anesthetic, has trismus which makes intubation more difficult, has not been NPO and has a three times higher incidence of p ml ain less s ostoperative hemorrhage.
presents with several days of sore throat which has become dramatically worse over the last 24 to 48 hours. The patient has trouble swallowing even liquids and has a “hot potato” voice. On examination there is a moderate amount of trismus making it difficult to open the mouth. The uvula is swollen and displaced to the opposite side. The anterior tonsillar pillar is classically quite swollen and hides most of the involved tonsil which may have some exudate. The contralateral tonsil usuallyappears normal. If a CBC has been done, white cell counts are elevated and there is a left shift. A diagnosis is made when aspirating the peritonsillar space yields frank pus. This procedure is done by spraying the pharynx with topical anesthetic and then injecting the upper outer mucosa (X) and underlying space with stock solution of 1% xylocaine 1:100,000 epineprine. About 3 to 5 mls are used. After waiting about five minutes the peritonsillar space is then aspirated with an 18G needle on a 5 or 10 syringe. Often times in an ER setting this aspiration will provide temporary relief until more definitive drainage can be done. Once the abscess is drained the patient can usually be managed on oral p medications and antibiotics (penicillins or erythromycins) as an outpatient. The chance of developing a second PTA or going on to have chronic tonsil problems is about 15%. Therefore, we usually do not recommend a tonsillectomy un the patient has a second abscess or significant prior tonsillar problems. Tonsillectomy at the time of abscess drainage i usually avoided as the patient needs a general anesthetic, has trismus which makes intubation more difficult, has not been NPO and has a three times higher incidence of p ml ain less s ostoperative hemorrhage.
Peritonsillar Cellulitis presents very similarly to a peritonsillar abscess but has not quite gotten to the point of suppuration. The history and physical findings are similar but no pus is obtained on aspiration of the peritonsillar space. This patient will usually require several days of IV antibiotics (Unasyn, Kefzol, Cleocin) but may occasionally be managed by an initial IM injection (Rocephin, Kefzol) followed by PO penicillins and pain medications with follow up the next day. A dose or two of IV, IM, or PO steroids is often helpful and does not interfere with the immune response. Some patients with peritonsillar cellulitis will go on to frank abscess formation.
Mononucleosis is, as you know, a viral disease that affects lymphoid tissue and presents with URI type symptoms, lymphadenopathy, hepatosplenomegally, fatique and pharyngitis. At times the pharyngitis may be the predominate symptom. Here one sees a severe exudate on both tonsils that appear swollen but symmetric. The white count is usually minimally elevated and there is a lymphocytosis or monocytosis with a proliferation of atypical lymphocytes. Other blood tests for “Mono” are helpful but can be confusing. These are outlined and commented on below. Severe “monopharyngitis” usually requires a hospitalization while the diagnosis is being secured and the patient is given IV fluids and IV steroids (dexamethasone 10mg IV q 12H) and often IV antibiotics (Cleocin, ampicillin) to treat an associated secondary bacterial infection of the tonsils. Amoxicillin should be avoided in patients with mono or suspected mono as they will commonly develop a non-allergic rash. Of course, plenty of rest is essential.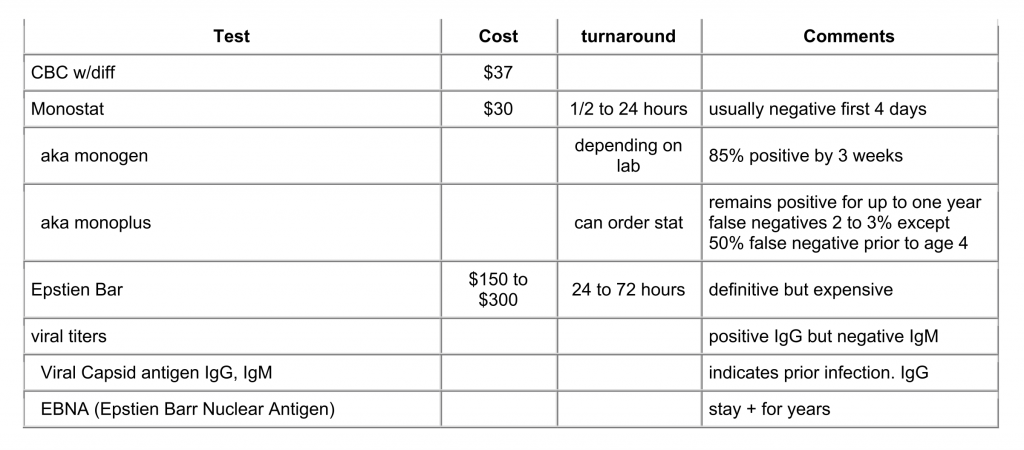
EBV early Antigen – this is a tumor marker for Nasopharyngeal carcinoma or chronic reactivated infections in imunocompromised patients -not on all panels.
Recommend: for inpatients or ER patients order monospot and “extra gold tube.” Call lab and see how long until it will be done, and if critical, order stat. If negative but suspicious for mono, then have gold tube run for EBV viral panel. For outpatients, consider ordering both if diagnostic dilemma since outpatient labs usually cannot hold a specimen. Balance this cost versus the possible need to have patient return for another blood draw.
Necrotizing Tonsillitis: This condition has a similar appearance to severe monopharyngitis with a thick necroticappearing bilateral tonsillar exudate, elevated WBC count and left shift but negative mono tests. Treatment is with I.V. antibiotics (Unasyn or ampicillin and Cleocin). Some patients can be tried on an initial IM dose of Rocephin or Kefzol with PO ampicillin and pain medicine.